Cardiovascular Diseases
Central pressures and cardiovascular risk
There are differences between peripheral and central points, such that systolic blood pressure is much higher in the brachial artery than in the central arteries, while diastolic pressure and mean pressure differ only slightly.
The blood pressure curves show differences depending on the points of the arterial tree where they are measured. There are differences between peripheral and central points, such that systolic blood pressure is much higher in the brachial artery than in the central arteries, while diastolic pressure and mean pressure differ only slightly. An elevation in central pressure, especially in systolic pressure, increases the left ventricle's afterload, causing a significant increase in cardiac workload, a stimulus that leads to the process of left ventricular hypertrophy and its eventual consequences, such as heart failure and myocardial ischemia.
Clinical and epidemiological studies have demonstrated the greater importance of systolic blood pressure over diastolic and mean blood pressure in evaluating cardiovascular risk, especially in the older adult population.1–4
However, the literature is still controversial, particularly regarding pulse pressure and systolic blood pressure in central and peripheral arteries, even when diastolic and systolic pressures appear to be equal.5,6,7
Such differences can lead to interpretative errors when analyzing myocardial oxygen consumption and left ventricular hypertrophy, as well as the analysis of the vasodilatory effects of different drugs. 8,9,10
The first hemodynamic studies conducted by catheterization in animals showed that pressures in the ascending aorta are quite similar to pressures within the left ventricle, but both are different from those measured in the brachial and radial arteries.20,21–23 These differences were attributed to the reflection waves and elasticity of the vessels, especially in young adults during tachycardia and physiological maneuvers such as the Valsalva maneuver.21,22 Other studies showed differences between the ascending aorta and the arteries of the upper limbs in elderly individuals, especially when experiencing tachycardia and/or hypotension or when under therapy with vasodilators. 6,11,24–26
More recently, Roman et al.27 demonstrated a greater correlation of cardiovascular risk with pressure in the ascending aorta compared to pressure obtained in the brachial artery.
Central arterial pressure can be obtained through non-invasive methods using new techniques that have generated great enthusiasm in evaluating central pressure in clinical practice. Two main methods are currently available: applanation tonometry, which estimates central pressure through non-invasive indirect recording (pressure recording on the arterial wall by a transducer); application of generalized transfer functions for indirect estimation of central aortic pressure waves, obtained through measurements made by tonometry in the brachial artery. However, both types of methodology present errors related to the calibration of the central pressure wave obtained through oscillometric measurement of the peripheral artery, demonstrating limiting but not restrictive factors for clinical application in different populations. Despite these limitations, some recent studies in specific populations have suggested that central pressure assessment may provide new perspectives and additional data for cardiovascular stratification in arterial hypertension.
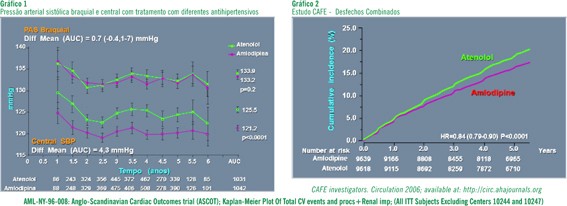
The CAFE clinical study compared the effects of treatment with different antihypertensives in combination on peripheral and central blood pressure (graphs 1 and 2). For obtaining central pressure, the function transfer methodology and applanation tonometry of the radial artery were used, and it was evidenced that reducing central BP leads to a greater decrease in cardiovascular risk than that observed with peripheral BP measurements (brachial artery). Also, the study showed that different antihypertensive drugs may have different responses on central blood pressure. Despite these data, the prognostic value of central aortic pressure measurements in large clinical studies remains unknown. Furthermore, adaptations in methodology for more accurate measurement of central BP are still necessary; however, when this becomes possible, data from large epidemiological studies and clinical trials will determine if optimizing assessment and reducing cardiovascular risk associated with increased BP will be feasible by analyzing local BP, where target organ damage or events occur, especially at the level of central arteries (aorta and carotids).